Macular Degeneration
Macular Degeneration: A Tough Nut to Crack
Macular degeneration is the most common cause of legal blindness (less than 20/200 in both eyes) among people over age 60 in the United States, afflicting millions. As the population ages, more and more will suffer from this serious disease. Despite some amazing advances in the treatment of macular degeneration, we still have a long way to go.
The macula is located in the middle of the retina. The center of the macula is the fovea, which controls central vision, the sharpest portion of the entire visual field. We use the macula and fovea for reading, cooking, watching TV, playing tennis, distinguishing colors, and just about everything that requires perception of fine details. Macular degeneration destroys the most important part of the retina. Macular degeneration generally does not affect peripheral vision, so patients do not go completely blind.
What Causes Macular Degeneration?
Macular degeneration is a diverse group of diseases, the most common of which is age-related macular degeneration (ARMD or AMD). AMD is classified into the “dry” and “wet” forms. The much more common dry form is characterized by degeneration of the macula and tissues that support the function of the macula. Dry macular degeneration does not respond to current available treatments. Fortunately, not everyone will suffer from significant vision loss.
Occasionally, dry macular degeneration transforms into the more serious wet form. Vision may deteriorate rapidly and suddenly from wet AMD. Abnormal blood vessels and membranes proliferate under the macula, causing bleeding, swelling, and eventually scarring. Depending on the location of the macular degeneration (whether it is directly under the very center of the macula) and the stage of the disease, different treatments may improve or stabilize vision.
How the disease actually occurs remains a mystery.
Risk Factors Include:
- Age. The risk of AMD rises steadily with age.
- Caucasian race, especially those with blue eyes.
- Smoking. Smokers have much higher risk of developing AMD and suffering vision loss from AMD
- Diet high in fat and cholesterol
- High blood pressure
- Genetics. The genetics appears very complicated. Although the risk of blood relatives of an AMD patient is higher than that of the general public, the risk cannot be easily quantified.
Symptoms
- Loss of central vision
- Distortion in vision (straight lines appear wavy)
- Areas near the center of vision appear shady or blurry
- May occur suddenly
- Often more pronounced in one eye initially. The likelihood the disease will affect the other eye depends on findings during examination. Ask your doctor to stratify your risk.
- Many people with mild AMD do not have symptoms.

How Do You Diagnosis Macular Degeneration?
Macular degeneration is diagnosed by examining the retina. The patient may be completely asymptomatic at the earlier stages of the disease. Frequently, ancillary testing such as optical coherence tomography (using light to scan the macula to obtain a high definition, cross-sectional picture) or fundus photography (a magnified color photograph of the macula) is taken in the office non-invasively to document the stage and severity of the disease. Occasionally, fluorescein angiography, which requires injection of a dye into the veins of the arm, followed by photos of the retina, is necessary to distinguish between the dry and the wet forms of the macular degeneration. Fluorescein angiography can also be used to identify the exact location of wet macular degeneration to pinpoint the best treatment.
How Does Macular Degeneration Get Treated?
There is currently no effective conventional remedy for dry macular degeneration, which generally progresses more slowly. Sometimes the wet form can be treated with laser if the abnormal membranes and blood vessels are located outside the central macula. The areas of abnormality are ablated with a carefully directed laser beam.
For an overwhelming majority of patients with wet macular degeneration, the current standard of care is an injection of medication into the eye. While not without discomfort, the injections are well-tolerated by most patients. Numerous clinical trials have confirmed the benefits of these medications (the most commonly used treatments now are Avastin, Lucentis, and Eylea) in treating active wet macular degeneration. However, they do not benefit every patient and often require ongoing treatment every few weeks. Treatment is often highly individualized, so discuss with your eye doctor about your specific situation. Finally, a treatment called photodynamic therapy may benefit some patients, but is uncommonly done today.
Prevention and Stabilizing Macular Degeneration
Because we don’t know exactly what causes AMD, there is no sure way to prevent the disease. However, you can improve the odds by:
- Quitting smoking.
- Controlling high blood pressure by exercise, diet, and medications.
- Avoiding excessive ultraviolet light (stay out of the sun or wear glasses with UV light protective coating).
- Consuming a healthy diet rich in fruits, vegetables, and dietary fiber. Restriction of animal fat and cholesterol may be helpful.
- Taking lutein, zeaxanthine, and/or the AREDS (Age-Related Eye Disease Study) formulas (AREDS I and AREDS II). Seek advice of your eye doctor and medical doctor before initiating these supplements, especially if you smoke or have a history of smoking.
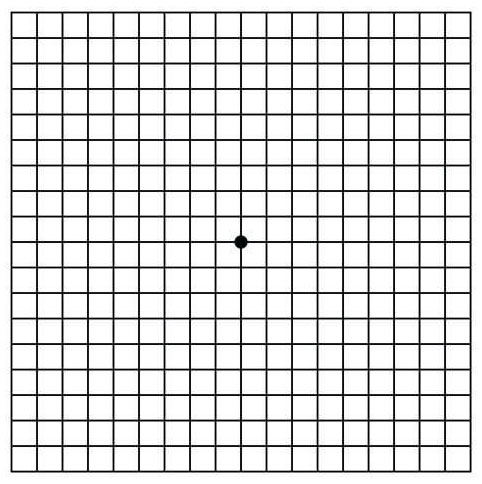
Once you have been diagnosed with macular degeneration, you should perform periodic Amsler grid exam:
- Hold the grid 14 inches away; put on reading glasses.
- Cover one eye.
- Focus on the black dot in the center of the grid.
- If any areas on the grid are hazy, black, distorted, or discolored, or if any lines are crooked, or if the exam appears to have changed since the last time, notify your doctor.
- Repeat with the other eye.